PCOS insulin resistance treatment: the complete guide
PCOS is very often accompanied by insulin resistance, which maintains a vicious cycle of hyperinsulinemia, excess androgens and symptoms (acne, irregular cycles, hirsutism...). Treatment is based mainly on lifestyle: a diet with a low glycemic load, regular physical activity and better stress and sleep management. Metformin may improve insulin sensitivity but the article advises keeping it as a last resort, after natural approaches.
.png)
- Publié le01.02.2026
.png) Modifié le01.02.2026
Modifié le01.02.2026
Faced with insulin resistance in the context of PCOS, the idea is not to look for a miracle solution, but rather to build a global and coherent strategy. We will try to restore the sensitivity of cells to insulin to finally break this vicious hormonal cycle that maintains the symptoms. The approach is based on a combined approach, where each element reinforces the others.
Above all, it is a question of adapting your lifestyle (diet, physical activity), a base sometimes supplemented by a drug therapy such as metformin and, in some cases, by dietary supplements well-chosen to improve insulin sensitivity and help regulate cycles.
The pillars of treatment for insulin resistance and PCOS
Managing insulin resistance associated with polycystic ovary syndrome (PCOS) is a marathon, not a sprint. The objective is simple in theory, but requires consistency: to make your cells receptive to insulin again. It's the key to breaking the vicious cycle that upsets your hormones and makes symptoms worse. This approach is based on three fundamental and complementary pillars.
A multi-level approach
The first pillar, and undoubtedly the most powerful, is the adjustment of your lifestyle. This includes targeted dietary changes and regular physical activity. Far from being a punitive diet, it's more about adopting new, sustainable habits to maintain stable blood sugar levels. It's the foundation for everything else.
Then comes the second pillar: medication options. When lifestyle efforts are not enough to rebalance everything, a doctor may prescribe treatments such as metformin. This medication is well known to help the body better manage blood sugar and, in turn, decrease the excessive production of androgens that is so typical of PCOS.
Finally, the third pillar is targeted support via dietary supplements. Some molecules, such as myo-inositol, have shown really interesting results in improving the work of insulin at the cellular level. This is a great help, but should always be discussed with a health professional.
In short
The management of insulin resistance in PCOS is a 360° strategy. It combines lifestyle (diet and sport), medication if necessary (such as metformin) and support through targeted food supplements. This integrated approach is the key to regaining control of your hormonal balance.
We strongly recommend that you choose natural solutions and avoid Metformin. It should only come in extreme cases, after trying the other solutions. We are just talking about it in theepisode 5 of No Rules PCOS.
.png)
The link between PCOS and insulin resistance: we decode
To act on the PCOS and insulin resistance, treatment It starts with understanding what is going on in our body. The bond between the two is so strong that they maintain each other, much like a vicious circle. To see more clearly, let's take a simple image.
Imagine that your body is a very active city. Each cell is a house that needs energy to function. This energy is the sugar (glucose) that circulates in the blood. And for this sugar to enter homes, a key is needed: that's the role of insulin, a hormone made by the pancreas.
When locks start to rust
Normally, after a meal, the pancreas releases just enough insulin to open cell doors and let sugar in. Blood sugar levels (blood sugar) drop and everything returns to normal. Simple.
But when there is insulin resistance, it's as if the door locks were a bit rusty.
No matter how hard the keys (insulin) try, they struggle to open the doors. The sugar therefore remains stuck outside, in the blood, and the blood sugar remains too high. The body sounds the alarm, and the pancreas, in a panic, starts producing a huge bunch of keys in an attempt to force a few locks. This phenomenon has a name: hyperinsulinemia. It is an excess of insulin that is constantly circulating. And that's where the direct link to PCOS comes in.
The impact of this excess insulin on the ovaries
This influx of insulin sends the wrong signals to other organs, especially to the ovaries. Normally, the ovaries produce a small amount of male hormones, androgens (such as testosterone). But under the effect of this hyperinsulinemia, they are overstimulated and start to produce far too much.
This hormonal imbalance is really the core of the problem in PCOS. This excess of androgens is directly responsible for many symptoms that you may be familiar with: irregular or absent cycles, persistent acne, hirsutism (hairs that grow on the face or body) or even hair loss.
The vicious circle is then in place:
- The cells are resistant to insulin.
- The pancreas compensates by producing more insulin (hyperinsulinemia).
- Excess insulin over-stimulates the ovaries, which make too many androgens.
- Excess androgens worsen PCOS symptoms and may even increase insulin resistance.
It is estimated that between 65 and 95% of women with PCOS have some form of insulin resistance, even without being overweight. For this reason, attacking insulin is often the keystone of management.
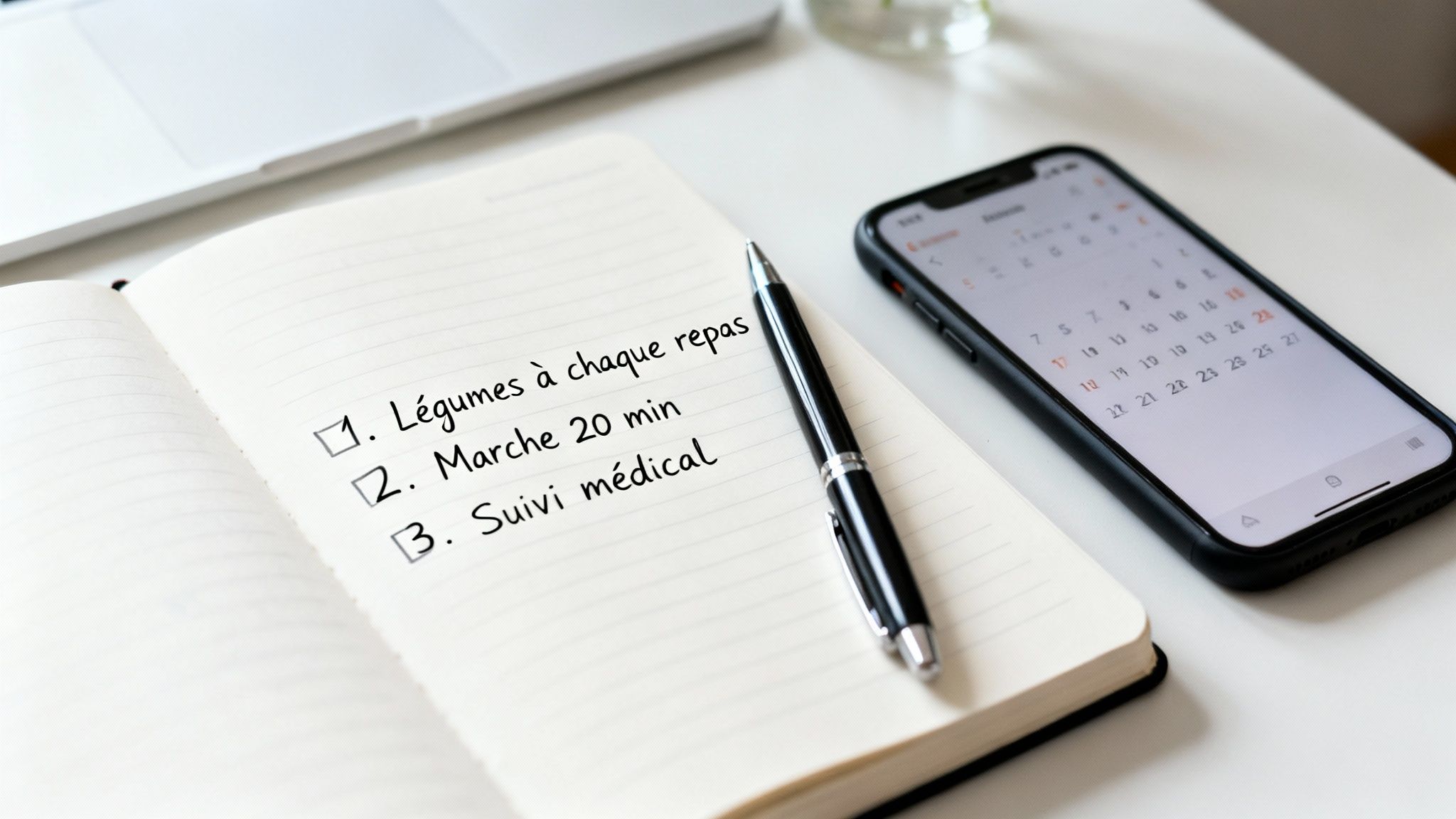
To visualize solutions, this illustration shows the three main pillars of treatment.
It is clear that the strategy is based on a combined approach: lifestyle, medications and supplements. To explore these topics, feel free to consult our resources dedicated to PCOS on Reflet and above all, join our free course dedicated to PCOS. Understanding this mechanism makes it possible to understand why the solutions do not only target the symptoms (such as acne), but also their root cause: this metabolic disorder.
Establishing an anti-insulin resistance lifestyle
Faced with insulin resistance, your lifestyle is by far the most powerful lever you have in your hands. Far from being a constraint, it is a great opportunity to regain control by acting on three fundamental pillars: your diet, your physical activity and your inner balance.
These three elements work hand in hand to “re-educate” your cells. The idea is to reteach them to listen to insulin messages. It is an active, caring approach, which forms the basis of everything treatment of insulin resistance associated with PCOS.

Food, your best ally in stabilizing blood sugar
The number one goal is not to get yourself into a frustrating restrictive diet. Rather, it is a question of adopting a diet with a low glycemic load. Clearly, we will favor foods that release their sugar slowly into the bloodstream, to avoid the glycemic roller coaster that forces your pancreas to overproduce insulin.
Think of your blood sugar as the water level in a bathtub. Fast sugars are like turning on the faucet all the way: the water rises sharply. Foods with a low glycemic load are a constant stream of water: the level remains stable and manageable.
Some concrete ways to take action:
- Fill half of your plate with vegetables: Broccoli, spinach, green beans, zucchini... They are full of fibers, which act as a brake on the absorption of sugars.
- Include a protein source in every meal: Chicken, fish, eggs, but also lentils or chickpeas. Protein calms and helps keep blood sugar levels stable.
- Choose good fats: Think avocado, olive oil, walnuts, almonds, or even fatty fish like sardines. They are anti-inflammatory and essential for your hormonal balance.
- Choose complex carbohydrates: Quinoa, brown rice, sweet potatoes, whole wheat sourdough bread... They are digested much more slowly than their refined cousins (white bread, white pasta, etc.).
- Avoid sugar in the morning : the insulin peak mostly takes place in the morning so it's a good thing to eat salty when you wake up.
A simple tip: never eat a carb by itself. Always accompany your fruit with a handful of almonds, or your wholemeal bread slice with a slice of ham or avocado. This small combination changes everything and slows the rise in your blood sugar considerably.
Moreover, this approach is a cornerstone of overall hormonal balance. To dig deeper into the subject, you can take a look at our guide on the link between nutrition and female fertility.
Physical activity to wake up your cells
Sport is a real treatment for insulin resistance. When you move, your muscles need energy. They then become able to fetch sugar directly from the blood, even with very little insulin. It's a bit as if sport gave them a go-to for glucose.
For maximum efficiency, the ideal is to combine two types of efforts.
- Cardio (endurance): It boosts heart health and burns glucose while you work out.
- Muscle building: It increases your muscle mass. And the more muscle you have, the more “garages” you have to store sugar, which helps keep blood sugar levels low.
Ideas to get you started:
- Fast walking: A simple stroll of 20 to 30 minutes After lunch can do wonders for your blood sugar levels in the afternoon.
- Swimming or biking: Activities that are gentle on the joints but extremely effective for the cardiovascular system.
- Pilates or dynamic yoga: They strengthen muscles deeply, improve posture and help better manage stress.
- Strength training: No need to lift tons! Exercises with light weights or simply with body weight (squats, lunges, push-ups) are already extremely beneficial.
There is no “best” sport. The most important thing is to find an activity that you really enjoy, in order to be able to maintain it over the long term. Aim for a consistency of 2 to 3 sessions per week.
Stress and sleep management, the pillar too often forgotten
Chronic stress and lack of sleep are real saboteurs in the fight against insulin resistance. Why? Because they cause your rate of cortisol, the stress hormone. When cortisol is consistently high, it tells your body to release sugar into the bloodstream to deal with an imaginary “danger.”
This sugar released all the time keeps your blood sugar levels high and exhausts your pancreas, which is running at full speed to produce insulin. It's a vicious cycle. Poor sleep has exactly the same effect. Taking care of your nervous system is therefore a non-negotiable step.
Concrete solutions to regain balance:
- Heart coherence: Take 3 to 5 minutes, several times a day, to breathe calmly: inhale for 5 seconds, then exhale for 5 seconds.
- Set up a sleep ritual: Try to go to bed and wake up at fixed times. Avoid screens for at least an hour before going to sleep and prefer quiet activities like reading.
- Take in the daylight: A small amount of exposure to natural light in the morning helps keep your body clock in sync for the whole day.
- Plan relaxing activities: Incorporate moments into your week that really relax you: a hot bath, listening to music, a walk in nature...
In short
To act effectively on insulin resistance in PCOS, your lifestyle is your first treatment. In practice, this means: composing a plate with a low glycemic load, moving by combining cardio and muscle building, and giving real importance to managing your stress and the quality of your sleep. These concrete actions make it possible to restore the sensitivity of your cells to insulin and to regain control of your hormonal balance.
With Reflet you have two options:
- Either join The free course dedicated to PCOS : you will then get the names of local professionals, concrete advice and access to the Reflet community dedicated to PCOS;
- Or, buy directly the Program Without Rules PCOS, where you will have concrete answers and an action plan dedicated to your PCOS.
Metformin and other drug treatments
When a healthier lifestyle, while absolutely essential, is not enough to set the hormonal record straight, a medical boost may be considered. It is an additional lever, often decisive, in the context of a treatment for PCOS and insulin resistance.
The medication that is most often found on a prescription is metformin. Historically known for treating type 2 diabetes, her talent for improving insulin sensitivity makes her an ally of choice for many women affected by PCOS.
How does metformin work
To fully understand what metformin does, think of it as a smart regulator that works on multiple fronts to calm your blood sugar levels. It doesn't force your body to make more insulin; rather, it helps your body make better use of the insulin that's already there.
Its mechanism is quite simple and comes down to two main actions:
- It calms the liver: Your liver has the ability to make and release sugar into the bloodstream. Metformin whispers to him to slow down this production, especially at night.
- It gives a helping hand to the muscles: It increases the sensitivity of muscle cells to insulin. To put it simply, it “ungrips” slightly rusty locks so that the keys (insulin) can open the doors again and let the sugar in.
This double effect makes it possible to reduce hyperinsulinemia, the famous excess of insulin that overstimulates the ovaries and feeds the vicious circle of PCOS.
By directly addressing the metabolic cause, metformin does more than just mask symptoms. It helps to restore a deeper hormonal balance by getting to the root of the problem: insulin resistance.
It is strongly recommended to take metformin as a last resort and to favor natural solutions such as food, sport or dietary supplements. Also, we recommend that you watch the Reflet Sans Rules PCOS program before taking Metformin.
Beyond metformin: what are the other options?
Even if metformin is often the first option on the table, other drug options can be explored, always within the framework of rigorous medical monitoring.
We are hearing more and more about GLP-1 agonists (like liraglutide or semaglutide). These are newer medications that help regulate blood sugar levels while promoting weight loss, a factor that is often linked to insulin resistance. Other molecules, such as Glitazones, can also improve insulin sensitivity, but they are used more rarely because of their potential side effects.
The choice of treatment will depend on your profile, symptoms, possible pregnancy plans, and overall health. An in-depth discussion with a specialist is therefore essential. To find your way around, it is often very useful to consult PCOS specialists who have an overall vision of care.
Building your personalized action plan
Moving from knowledge to action is where it all comes into play and it's exactly where Reflet intervenes. Knowing what to do is one thing, but managing to integrate it sustainably into your daily life is another. Here, I guide you step by step to build a tailor-made, caring and above all, realistic strategy to live better with your insulin resistance linked to PCOS.
The objective? Above all, not to revolutionize everything overnight, but rather to initiate a positive movement. This course is a marathon, not a sprint. Every step, even the smallest, is a victory.
Step 1: Surround yourself with the right team
You are not alone in this adventure. Trying to manage everything without support can be exhausting and even counterproductive. The very first action is therefore to put together your dream team.
This team is your base. Each member brings their expertise for comprehensive, 360-degree care:
- Your primary physician or endocrinologist: He will be the one who will make a complete diagnosis, prescribe the necessary blood tests, and can discuss medication options, such as metformin, with you.
- Your gynecologist or midwife: He or she will support you on everything related to your reproductive health, the regularity of your cycles and a possible pregnancy project.
- A dietitian-nutritionist specialized in: It is a key ally in transforming the main principles of a low glycemic diet into concrete, gourmet meals that adapt to your life.
Never underestimate the power of personalized support. A team that communicates well will help you see things more clearly, stay motivated, and adjust the strategy based on your progress and how you feel.
If you don't have the contacts of the right health professionals, join the Reflet course dedicated to PCOS.
Step 2: Set clear and achievable goals
The enthusiasm at the beginning sometimes pushes us to aim too high, too fast. Result? We are exhausted, we are discouraged. The key to success is Small steps method.
Start by choosing one or two goals very simple for the next two weeks. The idea is to create new habits that are so easy that it's almost impossible not to stick to them.
Some concrete examples to take action:
- Nutrition objective: “This week, I'm adding a portion of green vegetables to my breakfast every day.” It's so much more accessible than wanting to change your whole diet all at once.
- Movement objective: “I'm going for a walk of 20 minutes right after lunch, three times this week.”
- Sleep objective: “I'm going to put my phone away from my bed 30 minutes before going to sleep, Monday to Friday.”
Pick a goal that seems simple to you and write it down. Once it has become a reflex, you can add a new one. That's how you build lasting changes.
Step 3: Learn to listen and adjust
Your body is your best guide. Managing PCOS and insulin resistance is not an exact science, and what works great for one person won't necessarily work for another.
Be patient and kind to yourself. There will be “no” days, and that's totally normal. The important thing is not to let go of everything. Keep a small notebook to write down how you feel: your energy level, the quality of your sleep, your mood... This will help you identify what really makes you feel good and adjust the situation.
Regular follow-up with your medical team is also essential to objectively assess your progress (via blood tests, for example) and adapt treatment if necessary. Each small success is a stone that you add to the building of your well-being.
In short: Your summary to take action
Managing insulin resistance in the context of PCOS is based on a comprehensive and coherent approach. The main objective is to restore the sensitivity of your cells to insulin to break the hormonal vicious cycle.
Here are the key points to remember:
- Understand the mechanism: Insulin resistance forces the pancreas to produce excess insulin (hyperinsulinemia), which overstimulates the ovaries and increases androgen production, making PCOS symptoms worse.
- Pillar 1: The Way of Life: It is your most powerful lever. Focus on a diet with a low glycemic load (rich in fiber, proteins and good fats), regular physical activity combining cardio and muscle building, and good stress and sleep management.
- Pillar 2: Drugs: If needed, metformin is the most common treatment. It helps to reduce the production of sugar by the liver and improves its use by the muscles. Medical follow-up is essential.
- Pillar 3: Complements: Inositols, chromium, magnesium and omega-3 can offer valuable metabolic support, always after advice from a health professional.
- Your Personalized Plan: Surround yourself with a team of professionals, set small achievable goals (e.g. adding vegetables to a meal, taking a 20-minute walk) and learn to listen to your body to adjust your strategy.
This integrated approach is the best way to regain control, regulate your cycles and significantly improve your quality of life.
Chez Reflet, our mission is to transform medical knowledge into concrete actions so that you can regain control over your health. Our video programs, validated by experts, are designed to help you understand and take concrete action on PCOS.
Do I have to stop eating sugar completely if I have PCOS?
Programs that could help
Les programmes qui peuvent vous aider
Do we freeze our oocytes?
Le Rubis is the first podcast dedicated to egg freezing. I answer all your questions about this journey, I wonder about the emotional impacts of this approach and I give you the keys to take action (or not), as long as it's your choice! If you asked yourself the question “Should I freeze my eggs?” Once in your life, Le Rubis is made for you. Available only in French speaking.
I discover the Ruby.png)




.webp)
.png)


.png)

