Better Eggs
Understanding your cycle and ovarian reserve in order to produce a quality oocyte
In episode 1, we discuss the basics of the cycle, why it is important for it to be healthy at all stages of life and what role hormones play.
Watch the sequel
- 🎬 Accès à 100% des vidéos
- 🔬 Recommandations scientifiques
- ✅ Conseils conrets et actionnables
- 💌 Communauté d'entraide
- 🎓 Pro de santé experte et diplômée
- 📆 Sans engagement
🔊 This program is an information program by a trained professional. This is generic advice and is not a personalized diagnosis. In all cases, we recommend that you be followed by a gynecologist and/or a midwife for individualized follow-up.
What you will learn in this episode
The impact of the cycle in preconception
- The 4 phases of the menstrual cycle (and why D1 = spotting)
- Ovarian reserve and the fact that oocyte maturation starts ~3 months before ovulation.
- Why a “good cycle” is a sign of good overall health
- How to identify ovulation (and a possible anovulatory cycle).
- The difference between a “normal” cycle and optimal cycle.
The key points of the menstrual cycle
- The cycle is orchestrated by the mastermind (FSH/LH) → ovaries → womb (endometrium)
- An ovulated oocyte Today has begun to mature about 3 months ago
- We can't Do not increase the number of oocytes entering a cycle; one can act on their quality (lifestyle, nutritional intake, sleep, stress)
- A cycle that “looks normal” (duration) is not always optimum (hormonal quality)
- Progesterone assays are done At D+7 (from ovulation), not always at J21
💡 Key figures
Ovarian reserve and oocyte maturation
Ovarian reserve is the stock of primary oocytes present in the ovaries. This stock is already there when the little girl is still in her mother's womb, and then it gradually decreases throughout life.
- With each cycle, groups of microscopic oocytes leave this reserve and begin to grow in size;
- This growth takes place by “cohorts”, under the influence of hormones sent by the brain;
- An oocyte that is ovulated today began to mature about 3 months earlier, taking advantage of hormones from several successive cycles.
Today, we do not know how to increase the number of oocytes that enter a cycle.
- We can influence quality (diet, sleep, stress, lifestyle).
- You cannot increase the number of oocytes available in each cycle.
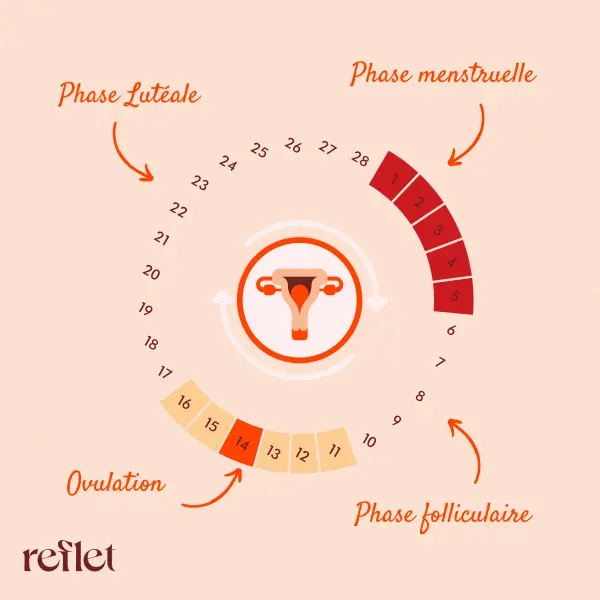
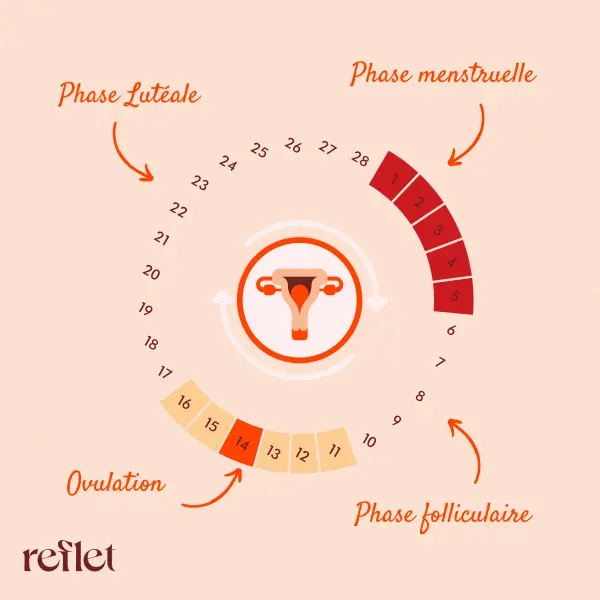
The main phases of the cycle
Carole then describes the main stages of the cycle.
- Menstrual phase:
- Starts on D-1, the first day of pure blood
- Corresponds to the evacuation of the endometrium from the previous cycle
- Follicular phase:
- In practice, it starts at the end of the previous cycle, but it is placed just after the rules to simplify.
- Under the action of FSH, a cohort of follicles begins to grow in size and produce estrogens.
- Its duration is very variable (around 10 to 18 days) and explains most of the variations in cycle length.
- Ovulation:
- When a follicle becomes dominant and produces enough estrogen, the brain triggers an LH surge (and a small FSH surge)
- This double peak causes the follicle to rupture and release the oocyte into the fallopian tube.
- Luteal phase:
- The emptied follicle is transformed into the corpus luteum, which secretes progesterone and estrogens.
- Progesterone stabilizes the endometrium and prepares the uterus for possible implantation
To check the quality of the luteal phase, Carole recalls that the progesterone dosage is done more on D+7 after ovulation than on a fixed day 21, because the length of the cycle varies between women.
🔎 Useful definitions
Amenorrhea: Amenorrhea is the absence of periods (also called menstruation) in a woman of menstrual age. It is normal during pregnancy, breastfeeding and during menopause. Otherwise, an assessment is necessary to find the cause.
Source: Ameli
____
Follicle: An ovarian follicle Is a spherical cluster of cells in the ovaries, containing the oocyte that is released during ovulation.
Source: Wikipedia
🎯 Actions concrètes
- Follow my cycle : note D1, duration, symptoms, and ovulation markers (“egg white” mucus, feeling, temperature if possible);
- Training in symptothermia is also an option, a Reflet program will obviously be created on this subject!
- Fertile window : try to have the ideal relationships of D-2 to D+1 (around ovulation);
- If repeated “weird” or anovulatory cycles : make a medical appointment with a midwife or gynecologist to explore causes;
- Targeted dosages : if necessary to assess the luteal phase, ask your doctor or midwife to check progesterone at D+7 (and not by default on J21);
- Oocyte quality starts long before conception: to work Right now (3 to 4 months before) on sleep, stress management, vitamin intake proteins and quality lipids (cell membranes need it).
- Remain pragmatic : we can't Do not increase the number of oocytes in a cycle, but we can optimize their quality by acting on what depends on us.
One thing is certain, we know that you can do it!
🔊 This program is an information program by a trained professional. This is generic advice and is not a personalized diagnosis. In all cases, we recommend that you be followed by a gynecologist and/or a midwife for individualized follow-up.
What you will learn in this episode
The impact of the cycle in preconception
- The 4 phases of the menstrual cycle (and why D1 = spotting)
- Ovarian reserve and the fact that oocyte maturation starts ~3 months before ovulation.
- Why a “good cycle” is a sign of good overall health
- How to identify ovulation (and a possible anovulatory cycle).
- The difference between a “normal” cycle and optimal cycle.
The key points of the menstrual cycle
- The cycle is orchestrated by the mastermind (FSH/LH) → ovaries → womb (endometrium)
- An ovulated oocyte Today has begun to mature about 3 months ago
- We can't Do not increase the number of oocytes entering a cycle; one can act on their quality (lifestyle, nutritional intake, sleep, stress)
- A cycle that “looks normal” (duration) is not always optimum (hormonal quality)
- Progesterone assays are done At D+7 (from ovulation), not always at J21
💡 Key figures
Ovarian reserve and oocyte maturation
Ovarian reserve is the stock of primary oocytes present in the ovaries. This stock is already there when the little girl is still in her mother's womb, and then it gradually decreases throughout life.
- With each cycle, groups of microscopic oocytes leave this reserve and begin to grow in size;
- This growth takes place by “cohorts”, under the influence of hormones sent by the brain;
- An oocyte that is ovulated today began to mature about 3 months earlier, taking advantage of hormones from several successive cycles.
Today, we do not know how to increase the number of oocytes that enter a cycle.
- We can influence quality (diet, sleep, stress, lifestyle).
- You cannot increase the number of oocytes available in each cycle.
The main phases of the cycle
Carole then describes the main stages of the cycle.
- Menstrual phase:
- Starts on D-1, the first day of pure blood
- Corresponds to the evacuation of the endometrium from the previous cycle
- Follicular phase:
- In practice, it starts at the end of the previous cycle, but it is placed just after the rules to simplify.
- Under the action of FSH, a cohort of follicles begins to grow in size and produce estrogens.
- Its duration is very variable (around 10 to 18 days) and explains most of the variations in cycle length.
- Ovulation:
- When a follicle becomes dominant and produces enough estrogen, the brain triggers an LH surge (and a small FSH surge)
- This double peak causes the follicle to rupture and release the oocyte into the fallopian tube.
- Luteal phase:
- The emptied follicle is transformed into the corpus luteum, which secretes progesterone and estrogens.
- Progesterone stabilizes the endometrium and prepares the uterus for possible implantation
To check the quality of the luteal phase, Carole recalls that the progesterone dosage is done more on D+7 after ovulation than on a fixed day 21, because the length of the cycle varies between women.
🎯 Concrete actions
- Follow my cycle : note D1, duration, symptoms, and ovulation markers (“egg white” mucus, feeling, temperature if possible);
- Training in symptothermia is also an option, a Reflet program will obviously be created on this subject!
- Fertile window : try to have the ideal relationships of D-2 to D+1 (around ovulation);
- If repeated “weird” or anovulatory cycles : make a medical appointment with a midwife or gynecologist to explore causes;
- Targeted dosages : if necessary to assess the luteal phase, ask your doctor or midwife to check progesterone at D+7 (and not by default on J21);
- Oocyte quality starts long before conception: to work Right now (3 to 4 months before) on sleep, stress management, vitamin intake proteins and quality lipids (cell membranes need it).
- Remain pragmatic : we can't Do not increase the number of oocytes in a cycle, but we can optimize their quality by acting on what depends on us.
One thing is certain, we know that you can do it!
.png)

.png)

